Special services
from the
andrological laboratory
The examination of the sperm cells (spermatozoa) of the man represents an important diagnostic step, which is crucial for the further course of fertility treatment and the planning of individual treatment. Therefore, the preparation of well-founded spermiograms as well as the effective processing and evaluation of the sperms in the context of fertility treatment is of utmost importance. A further focus of
the andrological laboratory is the freezing of sperm or testicular tissue and storage in liquid nitrogen (cryopreservation of sperm or testicular tissue).
Apparative and personnel equipment
In our own laboratory we have the possibility to determine a whole range of andrological examinations for you as quickly as possible. Thanks to our modern equipment we have the most results on the same day. The examinations are carried out by our qualified staff. The findings and evaluation of the results are carried out promptly by our experienced specialists directly in the fertility clinic. In a detailed discussion with you or the patient, we can start with the best possible treatment. For special questions, we also have qualified urological/andrological cooperation partners at our disposal. Rapid results guarantee optimal care and support therapy-relevant decisions before, during and after each treatment. This enables us to react quickly and precisely to any unevenness. As with all discussions and treatments with you, data protection has the highest priority in order to protect your privacy.
The diagnostic spermiogram
The first step in the assessment of male ejaculatory ability is an examination of the seminal fluid, also called ejaculate. The collection takes place after 2-5 days of abstinence by masturbation with timely analysis in the laboratory, which is why a collection in the donor room of the
fertility centre should be carried out. Due to biological fluctuations, it is advisable to carry out at least two sperm examinations every 8-12 weeks. The analysis is carried out according to the guidelines of the World Health Organization (WHO), whereby the concentration (number) of sperm in the ejaculate, its mobility (motility) and appearance (morpholgy) and other characteristics are assessed in a standardised way. After the ejaculate has been processed by centrifugation, a new analysis is carried out in order to be able to give you an adequate therapy recommendation.
The therapeutic spermiogram
The therapeutic spermiogram also analyses concentration, mobility and morphology. However, special attention is paid to the preparation of the sample in order to achieve the best results for the therapy on this day.
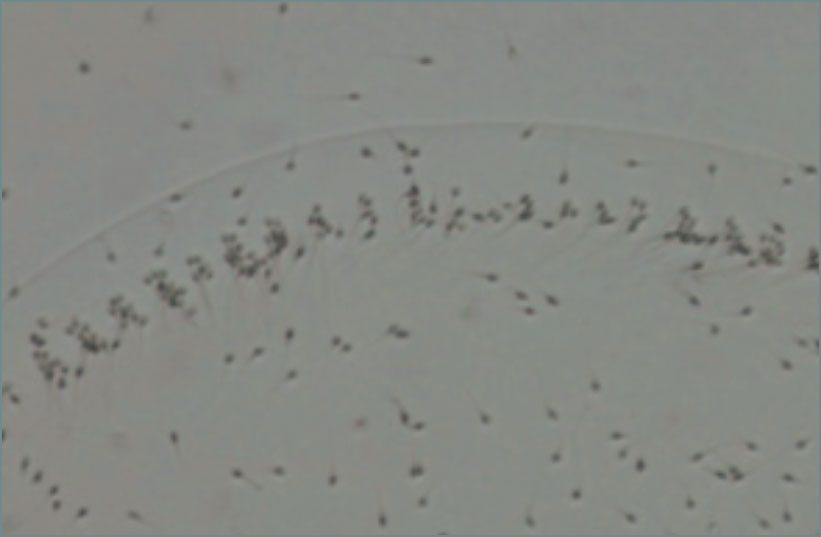
Examination of Vitality
If the motility of the sperm of a semen sample is reduced or if none of the sperm move, it is possible to find out whether the sperm are alive by staining them with an eosin solution. Because an immobile sperm does not have to be dead! And can therefore be used for fertility treatment. If the percentage of the actually dead (stained) sperm of a freshly collected sample (with abstinence period of 2 to 5 days) is higher than that of the living sperm, we recommend a urological examination to rule out inflammation or disease of the epididymis.
MAR (mixed antiglobulin reaction)
Sperm are “foreign bodies” for the male immune system. Therefore, they are separated from all others (especially the blood) and transported through the body. If this separation is reversed due to an injury, infection or other trauma, an antibody reaction occurs which causes the sperm to “clump” or can even damage the DNA of the sperm in various ways. These antisperm antibodies can be tested and, if the results are positive, the therapy can be adapted to the desired child.
Microbiological examination of the
Ejaculates – Ejaculate culture
In order to rule out a possible infection with fungi or bacteria (including chlamydia), which can occur with or without symptoms, the ejaculate can be examined microbiologically. If the results are positive, antibiotic therapy is recommended.
Laboratory chemical subsumations
of the ejaculate
Sperm are hardly or immobile during their formation. Only during their passage through the epididymis and vas deferens, past the prostate gland, the by the addition of various secretions (which form the seminal fluid), and of various substances (micronutrients, trace elements, etc.) in the secretions mobile. Due to a lower concentration or the absence of these substances can check the functioning of the organ or the gland that is adding and possibly treated.
DFI (DNA-Fragmentations-Index)
Sperm are also “fragile”. The main task of a sperm is to transport the DNA with the genetic information, which is located in the sperm head, into the egg cell. For this purpose, the sperm are normally given various nutrients and enzymes for the path. However, it remains unclear whether the DNA is intact or whether it arrives intact. Due to various causes, the DNA can be “broken”, i.e. it is present in fragments or it can “break” on its way to the egg cell. This reduces the probability of becoming pregnant or increases the risk of miscarriage. By determining the fragmentation rate of sperm in connection with the spermiogram, treatments which are less promising can be excluded from the outset, e.g. in the case of a high number of sperm which fragment on the way to the egg, the path should be “shortened”. Studies have shown that men can reduce the fragmentation index of their sperm by maintaining a healthy lifestyle with sufficient exercise and a balanced diet.
PICSI® – Physiological Intracytoplasmic Sperm Injection
Men with a low sperm count often have sperm without damaged DNA. Then ICSI treatment is usually necessary. These unsuitable sperm with impaired development and damage to the DNA can look normal and healthy. However, if you are selected for fertilisation, this may result in poor embryo quality and loss of pregnancy, a low fertilisation rate or failure to fertilise. In PICSI, the selection of sperm for injection into the egg is not primarily based on appearance (morphology), but on their biochemical maturity.
Fully mature sperm have sensors (receptors) on their heads for hyaluronic acid (hyaluran), which is an essential component of the egg shell (zona pellucida). PICSI is carried out using special shells coated with hyaloron gel, to which the mature sperm “bind”, while immature sperm continue to swim. In a second step, the bound sperm are assessed according to their morphology and the best are used for injection into the egg. Studies show that these sperm tend to have no or less DNA damage and can therefore lead to a higher fertilisation and pregnancy rate.
Cryopreservation of sperms
from the ejaculate
The technique of cryopreservation of sperm has been an established procedure for many years. Sperm cells are frozen and stored in liquid nitrogen at -196 degrees Celsius. Under these storage conditions, the sperm cells have an almost unlimited shelf life. It is possible to create a so-called sperm cell depot by donating several sperm donors in case of delivery difficulties or very low sperm concentrations or before a potentially germ cell damaging chemo- or radiotherapy. In the event that no sperm of one’s own is produced after the therapy has been completed, this depot can be used and with the help of artificial insemination measures an existing fertility wish can be realised.
Especially with testicular cancer, but also with leukaemias and lymphomas, limited fertility can often be found in the ejaculate even before treatment. Even in these cases, it makes sense to create a sperm cell depot, as there are usually still enough sperm for artificial insemination. In addition to chemotherapy and radiotherapy, fertility can also be impaired by surgery. Within the scope of a lymph node removal in the area of the pelvis, e.g. during operations on testicular tumours, damage to the nerves that control ejaculation can also occur in rare cases with gentle surgical techniques. Operations on the prostate or bladder can also impair the ability to ejaculate. In this case, testicular tissue could be surgically removed and stored deep-frozen in liquid nitrogen in order to carry out artificial insemination with isolated sperm if the patient later wishes to have children.
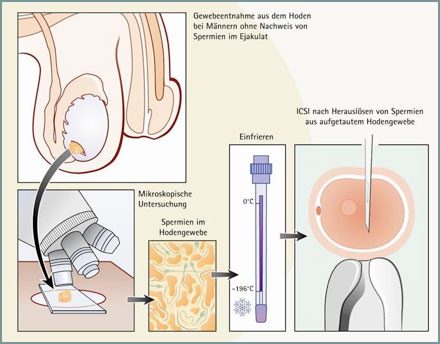
Azoospermia (MESA/TESE) – Freezing of sperm from testicular tissue (TESE)
TESE (testicular sperm extraction) is a well-established treatment method available for men who do not have sperm in their ejaculate or for whom it is not possible to release sperm. TESE is the extraction of sperm from the testicular tissue. In an outpatient procedure, several small tissue samples are surgically taken from the testicles under anaesthesia and then frozen in liquid nitrogen and stored. In the further course of the fertility treatment, sperm can be obtained from these samples after they have been thawed. This method has been used for many years, but the chances of success depend on whether there are enough fertile sperm in the testicular tissue at the time of freezing. This is analysed immediately after tissue removal. Artificial insemination can be performed from these spermatozoa at a later point in time.